Nephrotic syndrome
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case i have seen:
The youngest of 4 and working as a cashier patient reported to work as usual 2 weeks ago, when his friends asked if he overslept and developed a puffy face. Puzzled, the patient immediately saw himself in the mirror and noticed that he had periorbital edema under both eyes. He did not have any rash, lip swelling or difficulty in chewing or pain in jaws at that point. No history of wheeze or pain abdomen at that point. He said that after a few hours of work, the edema subsided spontaneously and the same sequence of events happend for the next 2 days. Sensing some problem, the patient quit work and returned to his hometown. The next day he noticed that he also started developing pedal edema, initially in the left ankle and gradually becoming bilateral. The edema progressively increased upto his knees over 3 days. He later developed distension of abdomen which was associated with early satiety. He denied constipation, vomiting, pain abdomen or fever. Distressed, the patient sought help with a local practitioner who prescribed a myriad of drugs, which he says did not do much to relieve his symptoms. A few days later, the patient also noticed that he was becoming breathless with minimal exertion. He says he couldn't even walk for a few yards before becoming breathless. He denied palpitations, syncope or presyncope, chest pain, cough or expectoration. He reported fatigue since the last 5 days.
He denies a history of sore throat, skin lesions, blurring of vision or pain in the eyes, no history of hemoptysis, upper respiratory tract symptoms or allergic symptoms. No history of night sweats or weight loss either. No history of dysuria or hematuria. He reports he had been having foamy urine for the past 2 weeks. No decreased urine output.
The patient's drug history is significant for using Nitrofurantoin for 1 week. He denies any recreational drug use or abuse. He denies previous sexual activity. No history of exposure to pets or domesticated animals. His past medical history is significant for Chickenpox at age of 12
The patient is keenly interested in knowing about his problem and wants a quick resolution so that he can get back
GENERAL EXAMINATION
Patient is conscious coherent cooperative moderately built and nourished
VITALS
BP-140/90
Pulse-92
Temp-afebrile
Spo2-96%at room air
Grbs-124mg /dl
RR-26cycles/min
No pallor icterus cyanosis clubbing lymphadenopathy
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM:
Shape of chest:normal
B/l air entry present
Absent breath sounds and stony dull note heard over the highlighted area suggestive of pleural effusion
Cvs EXAMINATION
S1 S2 heard
No raised jvp
PER ABDOMEN examination
Shape of abdomen - mild distended
Umbilicus-inverted
No organomegaly
Puddle sign-positive suggestive of mild ascitis
CNS EXAMINATION
Higher mental functions normal
All cranial nerves intact
Motor -intact
Sensory-intact
No cerebellar signs
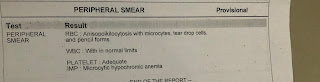
INVESTIGATIONS
Today’s urine sample shows absent RBC
RFT on 5/8/2020
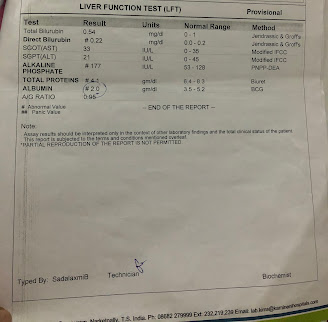
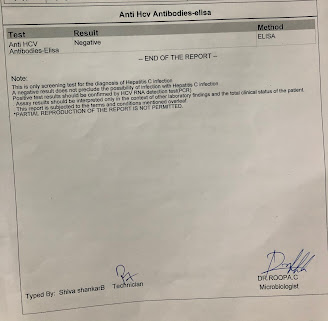
Reports on 6/08/2020
Thyroid profile
ABG report on 4/08/2020
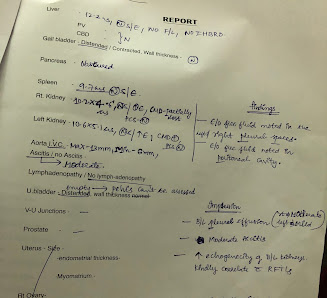
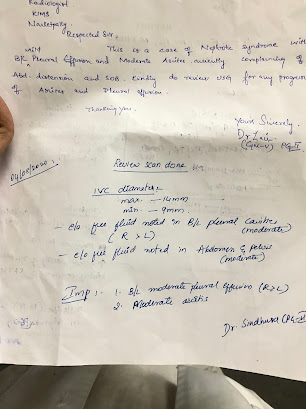
Review USG
ECG
Xray on 6/08/2020
PROBLEM REPRESENTATION
A 22 yr old previously healthy man presented with Anasarca, foamy urine and progressive shortness of breath since 2 weeks
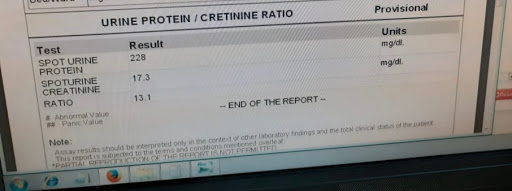
On examination he appeared mildly tachypneic at rest with pedal edema, ascites and pleural effusion. Laboratory investigations revealed a spot protein creatinine ratio of 10.7 and a mild hyponatremia at 131 meqs/L. A renal biopsy is planned and he is currently on diuretic therapy to relieve edema.
SOAP notes on 4/08/2020
22M with Nephrotic Syndrome
S - Feeling the same breathlessness (on leaving bed and going to washroom). Periorbital edema and pedal edema increased
O - Mildly tachypneic at rest with RR at 24. PR 97bpm and Spo2 98% on ambient air. He is afebrile with a BP of 100/70. Stony dull note with decreased to no breath sounds increased on both sides. Weight 64kgs (1 kilo increase).
A - Anasarca increasing. Pleural effusion has increased (clinically). Inadequate diuresis
P - Will require aggresive diuresis. Renal biopsy opinion today. A repeat Chest Xray and Serum albumin to gauge progress.
SOAP on 5/08/2020
22M with. Nephrotic Syndrome
S - Patient reports resolution of breathlessness. Distension of abdomen decreased. He reports some improvement in overall functional capacity.
O - BP at 120/90. PR at 90. RR at 18 and Spo2 on ambient air 98. Weight 60kgs
A - Patient did not reach adequate diuresis target today. He is currently on dual diuretics which needs to be gauged for their potency tomorrow. He also received Lasix and Albumin today at 4 pm.
P - Renal biopsy still the definitive investigation. Diuresis and target body weight likely to be reached in 2 days.
TREATMENT GIVEN
1)inj lasix 40 mg iv bd
2)inj optineuron 1 amp 100 ml NS iv over. 30 min
3)tab pantop 40 mg od
4) salt restriction diet < 4 mg
5)inj albumin 20% 100ml iv over 45min from 4/08/2020
6)inj metolazone 2.5 BD from 5/08/2020
7) tab telmisartan 40 mg OD on 6/08/2020
DIAGNOSIS
NEPHROTIC SYNDROME for evaluation
DISCUSSION
COHORT STUDY showing histological type of nephrotic syndrome
Adult patients aged above 12 years with nephrotic range proteinuria and disclosing no secondary causes for nephrotic syndrome were included in this study. Age, gender, duration and degree of proteinuria, hematuria, oliguria, hypertension, edema, pleural effusion, ascites, hemoglobin, total and differential count, urine albumin, urine sediment, 24-h urinary protein, renal function tests, serum cholesterol, serum albumin and ultrasound of the abdomen of these patients were studied.
We studied 86 patients who underwent renal biopsy in the nephrology unit of our hospital. Among them, 65 were found to have nephrotic syndrome and 50 met the selection criteria for this study. The mean age of the patients was 34 ± 14.7 years, and 35 (70%) were males. The histological subtypes found in our patients included minimal change disease (MCNS) [11 (22%) patients], focal segmental glomerulosclerosis (FSGS) (23 [46%] patients) and membranous glomerulonephritis (MN) [16 (46%) patients].
Macrohematuria was revealed in five out of a total of 50 patients, and the majority of the patients (80%) gave a history of passing frothy urine. The pattern of distribution of hypertension among the histological subtypes did not show significant differences. A key point we are getting here is - Hematuria can also occur in Nephrotic syndromes and also Hypertension can also occur in Nephrotic Syndromes. Again, textbook learning gone with the wind 🏁
Three of the 11 cases of MCNS, seven of the 23 cases of FSGS and four of the 16 cases of MN had hypertension. There were 23 (46%) patients who had ascites at the time of presentation; 15 of 23 (65%) cases of FSGS had ascites, four of 11 cases had MCNS and four of 16 cases had MN. Microhematuria was revealed in 13 out of 50 (26%) patients in this study; 11/13 of them had FSGS and 2/13 cases had MN.
Severe hypoalbuminemia (serum albumin <2.5 g/dL) was observed in 34 of 50 (68%) cases; seven of 11 cases of MCNS, 11 of 16 cases of MN and 16 of 23 cases of FSGS had severe hypoalbuminemia.
This is a Keralite study so I think the patient characteristics in this study could match our patient's.






















Comments
Post a Comment